6 Endocrine Foundations
Why Hormones Matter in Thermoregulation
Hormones significantly influence how the body senses and responds to heat. This influence becomes especially important during reproductive stages such as the menstrual cycle, pregnancy, and menopause. The endocrine system modulates thermoregulation to support reproductive physiology, but these adaptations can reduce thermal flexibility and increase vulnerability to heat exposure (Dervis et al., 2021).
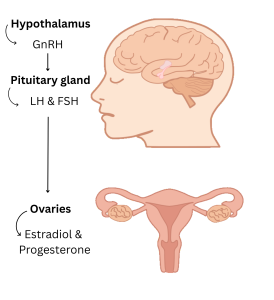
Understanding how estrogen and progesterone are regulated by the hypothalamic-pituitary-gonadal (HPG) axis helps explain why certain phases of the reproductive cycle are more thermally sensitive.
Estrogen: Supporting Heat Dissipation
Estradiol (E2), the dominant form of estrogen during reproductive years, promotes the body’s capacity to cool itself. It acts on the preoptic area of the hypothalamus to lower the thermoregulatory set point, allowing heat loss responses like sweating and vasodilation to activate at lower core temperatures (Silva & Boulant, 1986).
Estradiol enhances thermoregulation by:
-
Increasing cutaneous vasodilation, improving skin blood flow (Stachenfeld, 2008)
-
Enhancing sweat gland sensitivity (Charkoudian & Stachenfeld, 2016)
-
Upregulating protective proteins, including HSP72, under stress conditions (Hromadnikova et al., 2015)
These effects are most pronounced during the follicular phase of the menstrual cycle, when estradiol is high and progesterone is low.
Progesterone: Promoting Heat Retention
Progesterone, which rises after ovulation and remains elevated during pregnancy, has a thermogenic effect. It raises the core temperature set point by approximately 0.3 to 0.5°C, delaying the onset of heat-dissipating responses (Stachenfeld et al., 2000).
Key effects include:
-
Delaying sweating and vasodilation
-
Increasing core temperature during rest and sleep (Baker et al., 2001)
-
Enhancing thermal conservation, which may support early embryonic development
These changes help optimize the uterine environment but reduce tolerance to external heat, particularly in the luteal phase and during late pregnancy (Dervis et al., 2021).

Mechanisms of Steroid Hormone Action: Genomic and Non-Genomic Pathways
Steroid hormones exert their effects through two main mechanisms: genomic and non-genomic pathways. These distinct modes of action allow for both long-term physiological adaptations and rapid cellular responses to environmental stimuli, including changes in temperature.
Genomic Actions
In the genomic pathway, steroid hormones such as estradiol and progesterone diffuse through the cell membrane and bind to intracellular nuclear receptors. Once activated, these hormone–receptor complexes translocate to the nucleus, where they interact with specific DNA sequences to regulate gene transcription.
This process typically has a slower onset, requiring hours to days, but leads to sustained changes in protein expression. Genomic effects play a critical role in reproductive tissue development, immune modulation, and thermal adaptation over longer timeframes.
Non-Genomic Actions
In contrast, non-genomic effects are initiated at or near the cell surface. Steroid hormones can bind to membrane-associated receptors, including G protein–coupled receptors or membrane-localized variants of classical nuclear receptors. This activates intracellular signaling cascades that may involve kinases, second messengers, or ion channels.
These responses occur within seconds to minutes, influencing processes such as vascular tone, calcium signaling, and neuronal excitability. In the context of thermoregulation, non-genomic actions of estradiol and progesterone are thought to rapidly alter heat dissipation and core temperature regulation by modulating hypothalamic neurons and peripheral blood flow.
Integration and Implications
The dual nature of steroid hormone signaling allows for both rapid thermal adjustments and long-term homeostatic regulation. This is particularly relevant during phases of the reproductive cycle, pregnancy, and menopause, when shifts in hormone levels impact both the set point for thermoregulation and the efficiency of heat loss mechanisms.
The hypothalamic-pituitary-gonadal (HPG) axis integrates these hormonal signals with central thermoregulatory centers in the brain, coordinating reproductive function with the body’s ability to manage heat.
Summary
-
Estrogen enhances the body’s ability to dissipate heat. Progesterone has the opposite effect and supports heat retention.
-
The HPG axis integrates hormonal regulation with the brain regions that manage body temperature.
-
Steroid hormones influence physiology both through gene regulation and through rapid cellular responses.
References
Baker, F. C., Waner, J. I., Vieira, E. F., Taylor, S. R., Driver, H. S., & Mitchell, D. (2001). Sleep and 24‑hour body temperatures: A comparison in young men, naturally cycling women and women taking hormonal contraceptives. Journal of Physiology, 530(3), 565–574. https://doi.org/10.1111/j.1469-7793.2001.0565k.x
Baker, F. C., Waner, J. I., Vieira, E. F., Taylor, S. R., Driver, H. S., & Mitchell, D. (2001). [duplicate entry—omit duplicate in final list]
Charkoudian, N., & Stachenfeld, N. S. (2016). Sex hormone effects on autonomic mechanisms of thermoregulation in humans. Autonomic Neuroscience, 196, 75–80. https://doi.org/10.1016/j.autneu.2015.11.004
Kelly, M. J., Rønnekleiv, O. K., Ibrahim, N., Lagrange, A. H., & Wagner, E. J. (2002). Estrogen modulation of K⁺ channel activity in hypothalamic neurons involved in the control of the reproductive axis. Steroids, 67(6), 447–456. https://doi.org/10.1016/S0039-128X(01)00181-7
Silva, N. L., & Boulant, J. A. (1986). Effects of steroid hormones on thermosensitive neurons in hypothalamic tissue slices. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 250(3), R625–R632. https://doi.org/10.1152/ajpregu.1986.250.3.R625
Stachenfeld, N. S., Silva, C., & Keefe, D. L. (2000). Estrogen modifies the temperature effects of progesterone. Journal of Applied Physiology, 88(5), 1643–1649. https://doi.org/10.1152/jappl.2000.88.5.1643
Media Attributions
- The hypothalamic-pituitary-gonadal (HPG) axis and its role in hormonal regulation. © Sophie Cotton
- Effects of estrogen and progesterone on thermoregulatory set point
